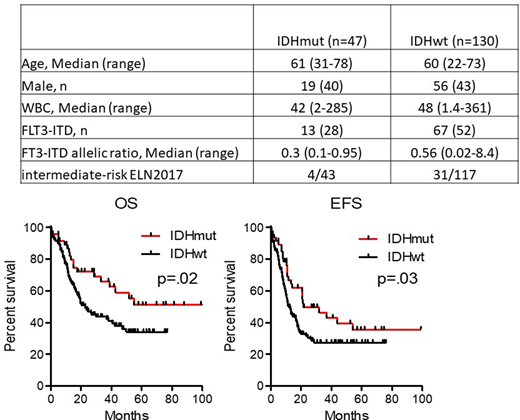
IDH mutations are strongly enriched in cytogenetically normal AML harboring NPM1 mutation (CN-NPM1mut-AML). The impact of these mutations on response to treatment is still a matter of debate. In the ELN 2017 classification, NPM1mut/FLT3-ITD allelic ratio >0.5 (FLT3-high) are considered intermediate-risk AML, whereas NPM1mut/ FLT3-ITD neg or <0.5 (FLT3-low) are low-risk. We aimed to evaluate the impact of IDH mutation in CN-NPM1mut-AML patients (pts) treated intensively. For this purpose, we retrospectively analyzed 177 CN-NPM1-AML pts from the Paoli-Calmettes Institute and from the French Innovative leukemia organization (FILO) databases who had received conventional intensive chemotherapy according to the FILO protocols (anthracycline-cytarabine based regimen for induction and High-intermediate dose cytarabine (HIDAC) for consolidation. Forty-seven (26%) AML pts had an IDH mutation -18 IDH1-R132 (10%), 27 IDH2-R140 (15%) and 2 IDH2-R172 (1%) - while 130 AML pts were IDHwt. Pts characteristics are presented in the Table.The complete response rate after one or two courses of chemotherapy (CR1) was 100% and 90% (p-value=.03) in the IDHmut and IDHwt groups, respectively. For pts in CR1, NPM1 molecular residual disease after the first consolidation (MRD2) was negative (>4 Log reduction) in 86% vs 53% of pts (p-value=.04). Nine (19%) and 24 (18%) pts received an allogeneic transplantation in CR1. The median time between CR1 and relapse was 11 months and 8 months, in IDHmut and IDHwt pts, respectively (p-value=.008). Day-100 non-relapse mortality was 8% and 12% respectively (p-value=ns). Median follow-up is 45 months (range, 2.4-115). Median EFS and OS are 21 months vs 12 months (p-value=.01) and 112 vs 23 months (p-value=.02), in the IDHmut vs IDHwt groups respectively (Figure). No survival differences were observed between IDH1mut and IDH2mut AML patients. Multivariate analyses with age>65, FLT3-high and IDHmut as covariates showed that IDHmut was independently associated with a higher EFS (HR=1.7, ranges 1.1-2.6) and OS (HR=1.7, ranges 1.1-2.7). Our results suggest that IDHmut is associated with a better response and a good disease control with high-dose chemotherapy. Nevertheless, some relapses still occur justifying the use of an IDH inhibitor combined with first-line chemotherapy or in a post-remission maintenance setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.